It is estimated that 400,000 children and adolescents develop cancer each year. This number is made up 76 different types of cancers with the most common being leukemia, brain, CNS and intracranial tumors and lymphomas (National Cancer Institute, 2024).
Approximately one-third of all children with cancer will be treated with radiotherapy either as a stand-alone treatment or combined with chemotherapy and/or surgery (Oswald, 2025).
Photons are the most commonly used form of radiation therapy in the treatment of childhood cancer. However, more focus is being given to protons and heavy ions due to the physical properties of these particles and their ability to reduce dose to healthy tissue and potentially reduce late effects, this is especially important in pediatric patients. However high costs and subsequent lack of accessibility continue to limit its use clinically despite encouraging dosimetric studies.
Radiotherapy accuracy is influenced significantly by a patient’s ability to remain completely still throughout treatment with the help of various immobilization devices including thermoplastic masks. Where radiotherapy treatments are becoming increasingly more complex and protons therapy taking longer than standard photon treatments, it can understandably be very difficult for children to stay completely immobilized and in isolation for prolonged periods of time. In some circumstances, general anesthetic or sedation is used to achieve this. Research suggests anywhere from 11-52% of patients require anesthesia for radiotherapy, with the need for it decreasing as the age of the child increases.
Anesthesia is associated with additional cost, logistical treatment challenges, increased resources, and health risks to the patient. It is estimated that the cost of daily anesthesia for a six-week course of radiotherapy treatment is in excess of $50,000 (Gutkins et al, 2023).
Research is increasingly focussed on how we can reduce the need for anesthesia as much as possible by working more closely with children to reduce their anxiety and increase their understanding to help improve compliance.
Play therapists
When assessing a child to determine anesthesia requirements, the child’s age, anticipated length of daily treatment, and additional medical, behavioral, and psychosocial needs are all considered. A play therapist plays a pivotal role in that assessment and in supporting the patient and their family throughout treatment, regardless of the anesthesia pathway they follow.
A play therapist incorporates age-related play, education, and coping techniques to help prepare patients and their families for treatment. They can provide psychoeducational intervention with play programs, interactive sessions, and pre-exposure therapy where patients can get familiar with staff, equipment, and the workflow of the radiotherapy department (Oswald et al, 2025).
Distraction
Audiovisual interventions have long been a staple method of increasing understanding of treatment and provide a distraction during treatment with the use of music, videos and intercom systems. As the technological world has developed, so has its role in supporting all cancer patients in terms of meeting informational needs. For younger patients, interactive educational tools, and virtual reality (VR) have been shown to reduce stress and anxiety. These tools are especially helpful with children under 7 years old, with research showing that this age group benefits most from visual preparation before treatment commences (Engvall, et al. (2018).
A study by Hiniker et al. (2017) found that 92% of patients did not require anesthesia after utilizing the AVATAR system, an audiovisual distraction-based system. Balazy et al. (2020) found that treatment time decreased from 36.7 minutes to 22.6 minutes with the use of this system. In one study, a 2-year-old was successfully treated without anesthesia using this system.
A study by Ritchie et al. (2024) investigated the intrafraction movement of children receiving radiotherapy awake with the help of audiovisual distraction and standard immobilization devices such as thermoplastic masks and vacuum bags. They found very few fractions in which more than minimal movement (>3mm for head and neck patients and >5mm for non-head and neck treatments) was detected. Where movement was detected, it was within typical PTV margins.
What the future holds
Upright radiotherapy is arguably the next great change in the delivery of radiotherapy treatment and there will always be circumstances where sedation or anesthesia is the safest option for a child receiving treatment. The question is whether it is possible to undertake this with a child in an upright position. Whilst it is feasible to treat a child upright and this has been successfully achieved in the clinical setting, intubation upright is rarely used clinically. However, a study by Turner et al. (2017) showed an 85.6% first-pass success rate when intubating a patient upright compared to 65.8% whilst the patient was supine. They predicted that upright intubation success rates would increase even further with more extensive training and experience. This suggests that anesthesia does not need to be a limiting factor in the widespread use of upright treatments for children.
Preliminary research into intrafraction movement and patient comfort amongst adults using Leo Cancer Care’s upright patient positioning system has shown patient preference to the upright position. They report feeling more comfortable breathing, they found it easier getting in and out of the system and felt more stable when compared to supine treatment. This study found less than 1mm intra-fraction motion for 80% of patients (Boisbouvier et al, 2022). Suggesting patients are comfortable and the system successfully stabilizes their position to deliver accurate and reproducible treatment.
This research was carried out at Centre Léon Bérard where they have also explored the use of hypnotherapy as an alternative to general anesthesia in the treatment of pediatric patients and they successfully saw a reduction in the need for general anesthetic when using rituals and hypnosis. They successfully treated half of all patients under 5 years old without the need for anesthesia regardless of whether treatment was high-technicity requiring optimal immobilization (Claude et al, 2016).
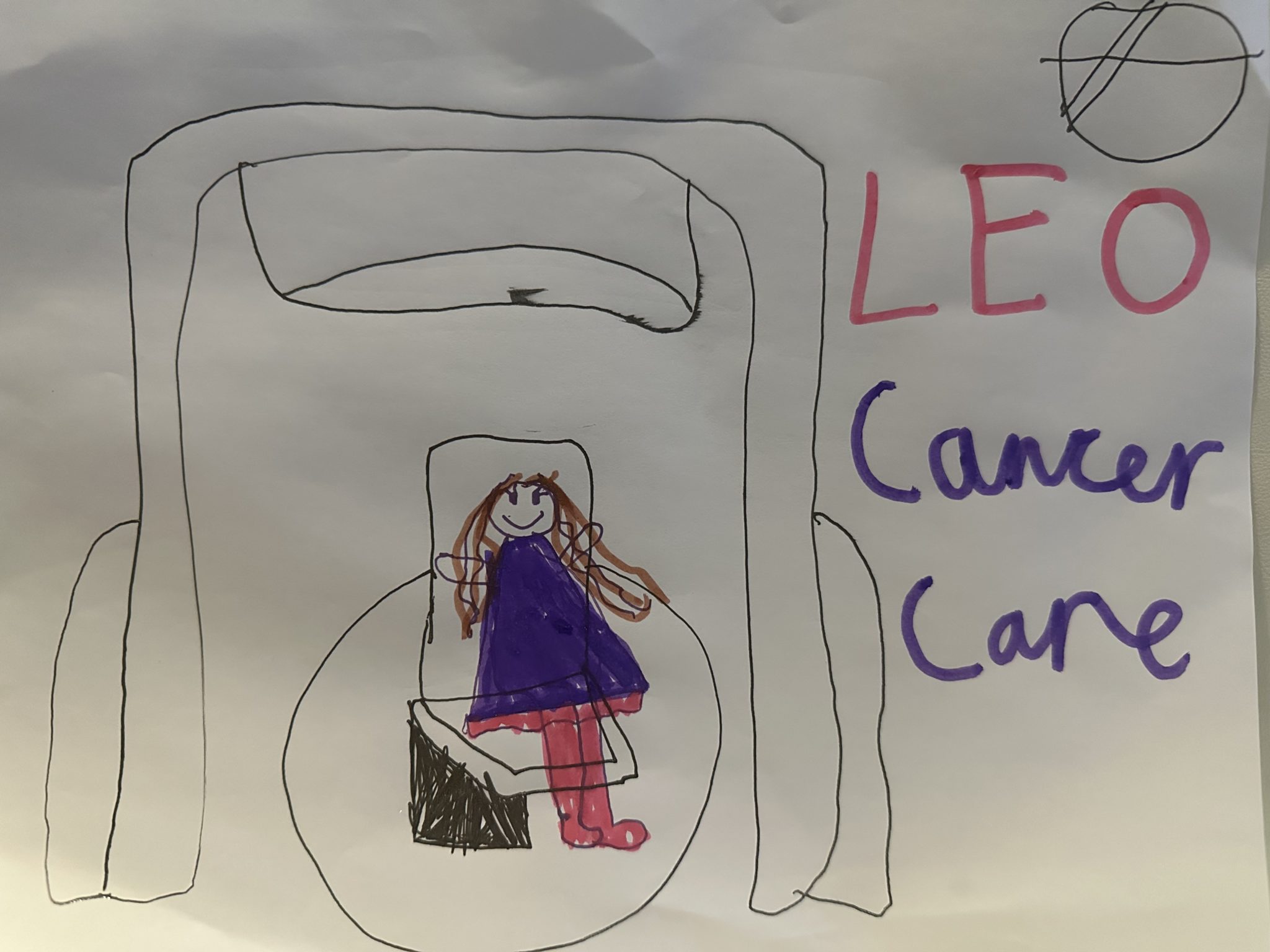
At Leo Cancer Care, we believe innovation goes beyond technology—it’s about transforming the patient experience. We are being proactive in exploring pediatric treatments reflecting our commitment to not only making radiotherapy more accessible but also ensuring a more comfortable, patient-centered approach for children.
As our technology matures, so does our dedication to making cancer treatment less intimidating and more effective for every patient. Children’s imaginations are restricted somewhat when having treatment in a supine position but in an upright position, why can’t their seat become a rocket ship, a throne, a racing car. If we make children the star of their own treatment with them right at the center then they could take us on a journey into space, a fairytale kingdom or winning 1st place at Formula 1.
The future of pediatric cancer care is evolving, and we hope to be a part of that evolution.
Please note: Leo Cancer Care technology is not yet clinically available
References
Claude, L., et al. Use of hypnosis in radiotherapy as an alternative to general anesthesia in pediatric radiation oncology. Bulletin du Cancer. 103, 11 (2016): 921-927
Engvall, G., Lindh, V., Mullaney, T. et al. Children’s experiences and responses towards an intervention for psychological preparation for radiotherapy. Radiat Oncol. 13, 9 (2018). https://doi.org/10.1186/s13014-017-0942-5
KE Balazy, PM Gutkin, L Skinner, et al. Impact of audiovisual-assisted therapeutic ambience in radiation therapy (AVATAR) on anesthesia use, payer charges, and treatment time in pediatric patients. Pract Radiat Oncol. 10 (2020), pp. e272-e279
Boisbouvier, S., et al. (2022). Upright patient positioning for pelvic radiotherapy treatments. Technical Innovations and Patient support in radiation oncology. 24. pp 124-130
SM Hiniker, K Bush, T Fowler, et al. Initial clinical outcomes of audiovisual-assisted therapeutic ambiance in radiation therapy (AVATAR). Pract Radiat Oncol. 7 (2017), pp. 311-318
Gutkins, P et al. Feasiblity of the Audio-Visual Assisted Therapeutic Ambience in Radiotherapy (AVATAR) System for Anesthesia Avoidance in Pediatric Patients: A Multicenter Trail. International Journal of Radiation Oncology Biology Physics. 117:1, 2023. 96-104
National Cancer Institute. Childhood Cancers. 2024. Available at: https://www.cancer.gov/types/childhood-cancers#:~:text=The%20most%20common%20types%20of,certain%20types%20of%20childhood%20cancer.
Oswald, L., Al-Kadhimi, S., Thorp, N. Anaesthesia for paediatric radiotherapy: A narrative review. Anaesthesia. 2025. 80(2) 44-53
RN Prasad, S Baliga, J Banner, et al. Radiation therapy without anesthesia for a 2-year-old child using audio-visual assisted therapeutic ambience in radiation therapy (AVATAR). Pract Radiat Oncol. 12 (2022), pp. E216-e220
Turner, J et al. Feasibility of upright patient positioning and intubation success rates at two academic Eds. The American Journal of Emergency Medicine. 35(7). 2017. 986-992
Subscribe to our newsletter
STAY CONNECTED
Get the latest updates and exclusive offers delivered straight to your inbox
Subscribe