Arc therapy- where it all began
Modern conformal radiotherapy has changed the way we treat cancer for the better. Introducing techniques such as modulation, image guidance and motion management have all improved dose conformity, efficiency and reproducibility (Hunte et al, 2022). All of which have increased survival and reduced toxicity for patients.
Intensity modulated radiotherapy (IMRT) was postulated over 40 years ago by Brahme et al (1983) and has been heralded as one of the biggest advancements in radiation therapy since the introduction of computed tomography into treatment planning, which opened the doors for 3-dimensional information of the tumor and the surrounding soft tissue (Choo, 2018). IMRT successfully improved dosimetric sparing of healthy tissue surrounding the tumor and organs-at-risk (Loebner et al, 2024), this helped to reduce the toxicities which had historically restricted dose escalation and negatively impacted overall survival and quality of life.
The first intensity-modulated rotational therapy called tomotherapy, was proposed by Mackie et al in 1993 using rotational therapy and a binary multileaf collimator (MLC). Tomotherapy was first delivered by a NOMOS Peacock device using licenses for tomotherapy the invention of Mackie and colleagues (Carol, 1993).
Intensity modulated arc therapy (IMAT) was introduced by Yu in 1995 as a treatment delivery method that intended to compete and address some of the limitations of few-field IMRT, which was starting to be implemented (Palma et al, 2010) using custom compensators or MLCs that had entered the field for replacing field-shaping custom blocks.
It used fixed beam angles with a ‘step and shoot’ style of treatment delivery that can lengthen treatment times for patients depending on how many beam angles have been planned. IMAT used optimization methods developed with tomotherapy but used continuously rotational beams rather than static ones with MLCs, with the field intensity pattern being formed by continuously changing the position of multileaf collimators (Matuszak et al. 2010).
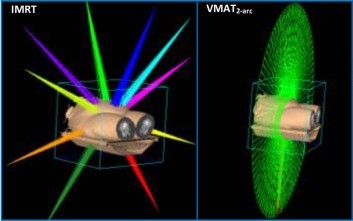
Volumetric modulated arc therapy (VMAT) was an implementation of IMAT first introduced by Varian in 2007.
It is difficult to ascertain precisely how many treatments use VMAT worldwide however, literature shows a strong preference for it as a treatment modality in place of 3DCRT (three-dimensional conformal radiotherapy). A study by Thanvi et al (2024) concluded that VMAT is more conformal than 3DCRT irrespective of the stage of the disease, type of disease and planned tumor volume. VMAT has a more homogenous dose than 3DCRT in all stages.
Dr Mehta at the Swedish Cancer Institute compared fixed-field and rotational IMRT plans for 100 patients when they initially VMAT and found that it was superior in 95% of cases. They have since repeated this study and found that for 99% of patients, VMAT offered a superior treatment plan in terms of fewer monitor units, better conformity and shorter treatment times.
Palma et al (2010) also highlighted a study which found that VMAT reduced treatment times from 20-30 minutes to 1.5-3 minutes and reduced monitor units by 50%.
Particle arc therapy
Arc therapy made a very quick impression on the photon treatment market however was slower to become established in the particle therapy sector. Initial questions were raised on whether the concept was counterintuitive as particle therapy is marketed as a treatment that can be delivered using fewer beams than conventional photon treatments as well as the concern of spreading the low-dose bath over a larger volume of healthy tissues.
Furthermore, to achieve arc treatment there needs to be a rotating component which is typically the gantry. For particle therapy this requires hundreds of tons of machinery to be moving whilst changing the magnet settings on the gantry magnets to maintain beam steering, achieving sub-millimetre accuracy to account for gantry sag and the changing direction of the Earth’s magnetic field which is a considerable engineering challenge (Mein et al, 2024).
Proton arc therapy was first discussed in 1995 by Deasy et al (Mein et al, 2024) and showed that for circular targets in a circular phantom that a near constant beam energy could be achieved by only modulating the beam current spatially. This method called “distal edge tracking” was never implemented because of the shape limitations but also because it would require the high LET Bragg peak to be at the edge of the treatment field which in turn requires accurate range calculations.
Since then, extensive research has since been carried out in support of this treatment modality in the effective treatment of specific disease sites with clear dosimetric advantages. Research has also identified the potential benefits of arc therapy within particle treatment with improved delivery workflow, decreased delivery time, increased tumor conformity and biophysical benefits (Li et al, 2019)
Mein (2024) looked at the potential benefits of arc therapy with heavier ions such as helium, carbons and oxygen, identifying the potential enhancement of linear energy transfer (LET) which will help to treat radio-resistant disease.
Another benefit of arc deliveries is that the use of high energy shoot-through beams to sharpen the beam edges is more feasible. This, in turn, will enable particle imaging measuring the energy of the particles traversing the patient.
The practicalities of introducing this as a mainstream treatment option is difficult due to the cost implications associated with large rotating gantries. Most of the 14 existing heavy ion therapy facilities utilize fixed-beam lines only, and there are only four heavy ion gantry systems in the world.
Li et al (2024) suggested an alternative economical approach to particle arc therapy, to focus on rotating the patient in front of a fixed beam rather than investing large capital in using a rotating gantry system. Chair systems were used in the preliminary years of particle therapy however their use was not extensive due to lack of commercial hardware that can set-up a patient to be fully relaxed and comfortable with minimal uncertainty as well as a lack of upright volumetric imaging capabilities (Volz et al, 2022). With industry interest growing in the revival of upright treatments and greater focus being spent on upright volumetric imaging, reproducibility, and patient comfort, this has become a viable option.
What impact could Leo Cancer Care have on particle arc therapy?
Leo Cancer Care’s upright technology could open the door to arc therapy for new and existing particle therapy facilities. The upright patient positioning system and upright CT scanner can be put in front of any existing fixed-beam radiation source. The patient positioning system can move in a continuous 360-degree motion, easily accommodating future particle therapy arc treatments. The upright CT scanner will allow for fully adaptive radiotherapy with daily diagnostic-quality imaging. The beam is fixed so there is no need to continuously correct the magnet steering to accommodate gantry sag and the changing direction of the Earth’s magnetic field. Fixed beam delivery nozzles can also be optimized for Arc specific type deliveries such as introducing fast multileaf collimators (MLCs) and in nozzle beam degraders.
Accessibility of arc therapy is improved because the compact nature of this system means it can fit into existing LINAC vaults so there is no need for extensive construction work to facilitate arc therapy in an existing particle therapy center or to build another cancer center if land is not available next to an existing center.
Preliminary research into the Leo Cancer Care upright patient positioning system suggests that reproducibility and stability are comparable to supine treatment systems and patients show a preference towards upright treatments from a comfort perspective, ease of breathing and ease of getting in and out of the system (Boisbouvier, 2022).
Early data indicates that the Iso centricity (rotation accuracy) of the Leo Cancer Care upright positioner will challenge current measurements from rotating gantries. Combining this with the fact that a stationary beam should be more stable, it is possible to believe that will facilitate simpler arc deliveries.
There is an ever-increasing demand on healthcare facilities to treat increasing numbers of patients with shorter waiting times and to provide patients with treatments that are efficient, evidence-based and that have minimal impact on patients’ quality of life. Particle arc therapy can achieve this however access to it is limited.
To meet the needs of patients, acceptance of innovation and new technology in the radiation oncology sector is essential and could increase global accessibility without compromising healthcare facilities economically. Upright radiotherapy is a perfect example of simplifying the currently complicated technology to unlock such innovations.
References
Brahme A, Roos J E and Lax I. Solution of an integral equation encountered in rotation therapy Phys. Med. Biol. 1982. 27 1221–9
Carol M P, et al. An automatic 3D treatment planning and implementation system for optimized conformal therapy. Three-Dimensional Treatment Planning ed P Minet (Geneva: WHO) 1993. pp 173–87
Cho B. Intensity-modulated radiation therapy: a review with a physics perspective. Radiat Oncol J. 2018 Mar;36(1):1-10. doi: 10.3857/roj.2018.00122.
Hunte SO, et al. Volumetric modulated arc therapy (VMAT): a review of clinical outcomes-what is the clinical evidence for the most effective implementation? Br J Radiol. 2022. 1;95(1136):20201289. doi: 10.1259/bjr.20201289.
Li, X., et al. 2. Treatment delivery. In: Mein, S., et al. Particle arc therapy: Status and potential. Radiotherapy and Oncology. 2024.199. https://doi.org/10.1016/j.radonc.2024.110434.
Loebner, H., et al. Robustness analysis of dynamic trajectory radiotherapy and volumetric modulated arc therapy plans for head and neck cancer. Physics and Imaging in Radiation Oncology, 2024. 30. https://doi.org/10.1016/j.phro.2024.100586.
Mackie TR, et al. Tomotherapy: A new concept in the delivery of dynamic conformal radiotherapy, Med. Phys. 1993. 20, 1709-1719
Massat, MB. VMAT: The next generation of IMRT. Applied Radiation Oncology. 2014. Available at: https://www.appliedradiationoncology.com/articles/vmat-the-next-generation-of-imrt
Matuszak, m., et al. Clinical Applications of Volumetric Modulated Arc Therapy. International Journal of Radiation Oncology Biology Physics. 2010. 77 (2): 608-616
Mein, S., et al. Particle arc therapy: Status and potential. Radiotherapy and Oncology. 2024.199. https://doi.org/10.1016/j.radonc.2024.110434.
Palma, D., et al. Chapter 7, New Developments in Arc radiation Therapy: A Review. Cancer Treatment Reviews 2010. 36(5):393-9
Thanvi, S., et al. Dosimetric Comparison of Conventional 3D-Conformal Radiotherapy (£DCRT) and Volumetric-Modulated Arc Therapy (VMAT) for Head and Neck Cancer. Asian Pacific Journal of Cancer Care. 2024. 9(1). Doi: 10.31557/apjcc.2024.9.1.49-53
Volz L, Sheng Y, Durante M, Graeff C (2022) Considerations for Upright Particle Therapy Patient Positioning and Associated Image Guidance. Front. Oncol. 12:930850. doi:10.3389/fonc.2022.930850
Subscribe to our newsletter
STAY CONNECTED
Get the latest updates and exclusive offers delivered straight to your inbox
Subscribe