The delivery of radiotherapy to the breast has long been subject to complexities and challenges due to the mobility and instability of breast tissue, the difficult treatment positions patients are often required to assume, and the close proximity of organs at risk, including the heart and lungs.
With the development of new technologies and methods of delivering treatment, including a resurgence of interest in upright radiotherapy, it is necessary to reassess whether these recognized challenges remain and how they might be better addressed.
To date, three key articles have focused on these challenges and explored whether upright treatment is feasible for this cohort of patients.
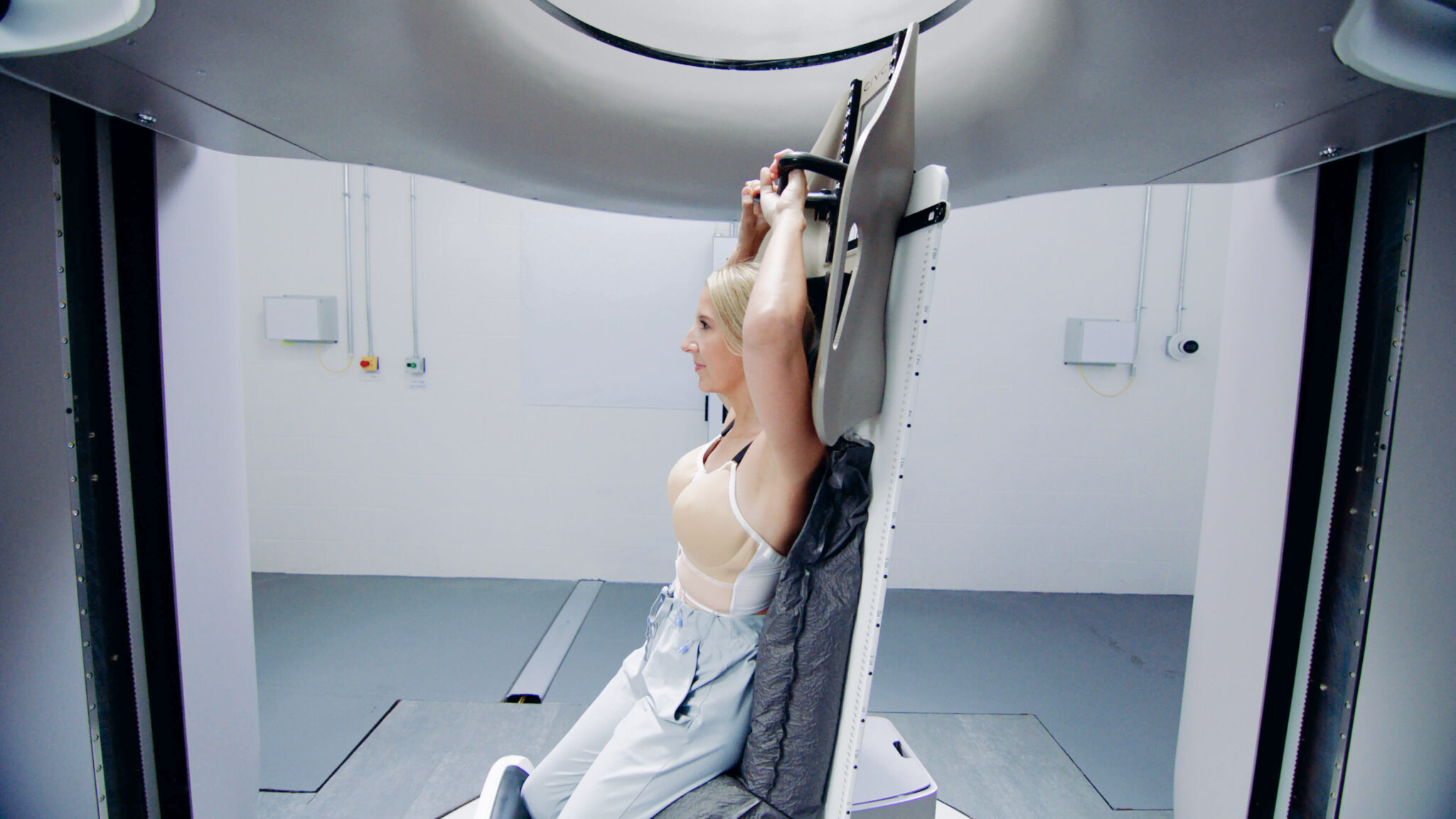
Boisbouvier et al. (1) were the first to investigate the feasibility of upright breast radiotherapy beyond a single patient case study (2), exploring the potential for highly precise curative treatments in an upright orientation. The study recruited 16 volunteers to assess two different radiotherapy bras, with a focus on patient comfort, treatment set-up reproducibility, and elimination of the infra-mammary skin fold (ISF).
The results showed that the majority of volunteers preferred the upright treatment position compared to the supine position. Participants found the radiotherapy bras easy to put on and comfortable to wear. From a clinical perspective, one of the bra designs successfully eliminated ISF in all volunteers, while the other did so in over half of the participants. The authors also noted that tilting the backrest further backwards helped to stretch the body and reduce abdominal tissue bunching beneath the breasts. Lower body reproducibility was consistent, with 81% of repeat set-ups matching within 3 mm in the breast region.
With patient positioning deemed feasible, subsequent research explored whether patients would actually want this change in treatment orientation. Ulman et al. (3) conducted a participatory co-design workshop involving people with lived experience of breast radiotherapy, healthcare practitioners, academics, and industry researchers. The workshop consisted of three stages:
(1) sharing experiences of supine treatment,
(2) identifying opportunities to improve the experience,
(3) exploring the upright experience.
During the final stage, participants sat in a demonstration upright patient positioning system and provided comfort scores and qualitative feedback.
The workshop highlighted how challenging the overall treatment pathway can be for patients, with radiotherapy representing just one component of that experience. Participants provided overwhelmingly positive feedback on the upright treatment option. Overall, 86% stated they would have preferred upright treatment, 77.8% found the upright position comfortable compared with 11.1% when lying down, and 66.7% reported feeling vulnerable in the supine position compared with only 11.1% in the upright position. These findings suggest that upright radiotherapy has the potential to improve not only physical comfort but also psychological wellbeing, by allowing patients to adopt a position in which they feel less vulnerable.

A final area of research explored by Sands et al (4) considered beam access for both photon and proton treatments and examined how arm positioning may influence treatment feasibility.
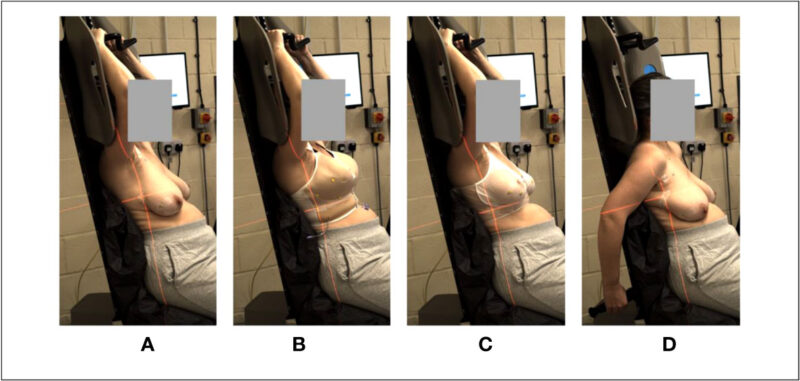
Three arm positions were investigated, with and without the use of a radiotherapy bra: arms up, arms by the side, and arms back. Optical surface scans were acquired, and beam access was evaluated for multiple regions of the breast, alongside field size measurements and assessment of the infra-mammary skin fold for each arm position. Participants also provided feedback on comfort for the different positions and were assessed for “unaided” reproducibility, evaluating their ability to position themselves accurately each day with minimal assistance from radiotherapy staff.
The results demonstrated that radiotherapy bras were effective in reducing infra-mammary skin folds. While clear advantages were observed, it was noted that the bra brought the breasts closer together, increasing the risk of contralateral breast clipping and therefore adding complexity to treatment planning. Use of the radiotherapy bra also allowed for a reduction in superior–inferior field lengths, which may help to reduce ipsilateral lung irradiation.
The three arm positions produced varied results. The arms-by-side position was unsuitable for photon beam treatments due to incompatibility with the lateral beam access required, although en-face proton fields were achievable. The arms-up position generally offered the greatest flexibility in beam access and the highest rate of successful treatment plans, particularly when used in conjunction with a radiotherapy bra. The arms-back position was unsuitable for 16% of photon plans due to obstruction of the desired beam path by the ipsilateral arm.
Participant feedback indicated that individuals felt comfortable and well supported in both the radiotherapy bras and the upright treatment position. Overall, participants demonstrated good levels of unaided reproducibility, with the ability to reposition themselves with sub-centimetre accuracy without assistance from the research team. This ‘hands-off’ approach to treatment set-up could help to increase patients’ sense of empowerment during radiotherapy.
Collectively, these three studies highlight the inherent complexity of breast cancer radiotherapy while demonstrating consistently positive outcomes in favor of an upright treatment position. Patients appear to prefer upright treatment in terms of comfort and reduced feelings of vulnerability.
The next step in this area of research will be the acquisition of CT imaging, or similar modalities, to assess how the required beam angles are affected by changes in internal anatomy, which has not yet been fully evaluated.
References
1. Boisbouvier, S., et al. Upright patient positioning for gantry-free breast radiotherapy: feasibility tests using a robotic chair and specialised bras. Frontiers in Oncology. 2023: 13. DOI=10.3389/fonc.2023.1250678
2. Mohiuddin MM, Zhang B, Tkaczuk K, Khakpour N. Upright, standing technique for breast radiation treatment in the morbidly-obese patient. Breast J. 2010;16(4):448-50. doi: 10.1111/j.1524-4741.2010.00932.x. Epub 2010 May 26. PMID: 20522098.
3. Ulman, J., et al. Exploring patient perceptions of the current breast radiotherapy pathway and a future upright radiotherapy solution. Radiography. 2025. 31(6) https://doi.org/10.1016/j.radi.2025.103157.
4. Sands, G., et al. Upright radiotherapy for breast cancer: a pre-clinical study considering photon and proton beam access, plus arm positioning. Frontiers in Oncology. 2025.15 . DOI=10.3389/fonc.2025.1668109
Subscribe to our newsletter
STAY CONNECTED
Get the latest updates and exclusive offers delivered straight to your inbox
Subscribe